05.23.19
People who experience anxiety symptoms might be helped by taking steps to regulate the microorganisms in their gut using probiotic and non-probiotic food and supplements, according to a review of studies published in the journal General Psychiatry.
Anxiety symptoms are common in people with mental diseases and a variety of physical disorders, especially in disorders that are related to stress. Previous studies have shown that as many as a third of people will be affected by anxiety symptoms during their lifetime.
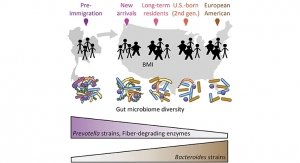
Increasingly, research has indicated that gut microbiota—the trillions of microorganisms in the gut which perform important functions in the immune system and metabolism by providing essential inflammatory mediators, nutrients and vitamins—can help regulate brain function through the so-called “gut-brain axis.”
Recent research also suggests that mental disorders could be treated by regulating the intestinal microbiota, but there is no specific evidence to support this.
Therefore, a team of researchers from the Shanghai Mental Health Center at Shanghai Jiao Tong University School of Medicine, set out to investigate if there was evidence to support improvement of anxiety symptoms by regulating intestinal microbiota.
They reviewed 21 studies that had looked at 1,503 people collectively.
Of the 21 studies, 14 had chosen probiotics as interventions to regulate intestinal microbiota (IRIFs), and seven chose non-probiotic ways, such as adjusting daily diets.
Probiotics are living organisms found naturally in some foods that are also known as “good” or “friendly” bacteria because they fight against harmful bacteria and prevent them from settling in the gut.
The researchers found that probiotic supplements in seven studies within their analysis contained only one kind of probiotic, two studies used a product that contained two kinds of probiotics, and the supplements used in the other five studies included at least three kinds.
Overall, 11 of the 21 studies showed a positive effect on anxiety symptoms by regulating intestinal microbiota, meaning that more than half (52%) of the studies showed this approach to be effective, although some studies that had used this approach did not find it worked.
Of the 14 studies that had used probiotics as the intervention, more than a third (36%) found them to be effective in reducing anxiety symptoms, while six of the remaining seven studies that had used non-probiotics as interventions found those to be effective—an 86% rate of effectiveness.
Some studies had used both the IRIF (interventions to regulate intestinal microbiota) approach and treatment as usual.
In the five studies that used treatment as usual and IRIF as interventions, only studies that had conducted non-probiotic ways got positive results, that showed a reduction in anxiety symptoms.
Non-probiotic interventions were also more effective in the studies that used IRIF alone.
In those studies only using IRIF, 80% were effective when using non-probiotic interventions, while only 45% were found to be effective when using probiotic ways.
The authors said one reason that non-probiotic interventions were significantly more effective than probiotic interventions was possibly due to the fact that changing diet (a diverse energy source) could have more of an impact on gut bacteria growth than introducing specific types of bacteria in a probiotic supplement.
Also, because some studies had involved introducing different types of probiotics, these could have fought against each other to work effectively, and many of the intervention times used might have been too short to significantly increase the abundance of the imported bacteria.
Most of the studies did not report serious adverse events, and only four studies reported mild adverse effects such as dry mouth and diarrhea.
This is an observational study, and as such, cannot establish cause. Indeed, the authors acknowledged some limitations, such as differences in study design, subjects, interventions and measurements, making the data unsuitable for further analysis.
Nevertheless, they said the overall quality of the 21 studies included was high.
The researchers concluded: “We find that more than half of the studies included showed it was positive to treat anxiety symptoms by regulation of intestinal microbiota.
“There are two kinds of interventions (probiotic and non-probiotic interventions) to regulate intestinal microbiota, and it should be highlighted that the non-probiotic interventions were more effective than the probiotic interventions. More studies are needed to clarify this conclusion since we still cannot run meta-analysis so far.”
They also suggested that, in addition to the use of psychiatric drugs for treatment, “we can also consider regulating intestinal flora to alleviate anxiety symptoms.”
Anxiety symptoms are common in people with mental diseases and a variety of physical disorders, especially in disorders that are related to stress. Previous studies have shown that as many as a third of people will be affected by anxiety symptoms during their lifetime.
Increasingly, research has indicated that gut microbiota—the trillions of microorganisms in the gut which perform important functions in the immune system and metabolism by providing essential inflammatory mediators, nutrients and vitamins—can help regulate brain function through the so-called “gut-brain axis.”
Recent research also suggests that mental disorders could be treated by regulating the intestinal microbiota, but there is no specific evidence to support this.
Therefore, a team of researchers from the Shanghai Mental Health Center at Shanghai Jiao Tong University School of Medicine, set out to investigate if there was evidence to support improvement of anxiety symptoms by regulating intestinal microbiota.
They reviewed 21 studies that had looked at 1,503 people collectively.
Of the 21 studies, 14 had chosen probiotics as interventions to regulate intestinal microbiota (IRIFs), and seven chose non-probiotic ways, such as adjusting daily diets.
Probiotics are living organisms found naturally in some foods that are also known as “good” or “friendly” bacteria because they fight against harmful bacteria and prevent them from settling in the gut.
The researchers found that probiotic supplements in seven studies within their analysis contained only one kind of probiotic, two studies used a product that contained two kinds of probiotics, and the supplements used in the other five studies included at least three kinds.
Overall, 11 of the 21 studies showed a positive effect on anxiety symptoms by regulating intestinal microbiota, meaning that more than half (52%) of the studies showed this approach to be effective, although some studies that had used this approach did not find it worked.
Of the 14 studies that had used probiotics as the intervention, more than a third (36%) found them to be effective in reducing anxiety symptoms, while six of the remaining seven studies that had used non-probiotics as interventions found those to be effective—an 86% rate of effectiveness.
Some studies had used both the IRIF (interventions to regulate intestinal microbiota) approach and treatment as usual.
In the five studies that used treatment as usual and IRIF as interventions, only studies that had conducted non-probiotic ways got positive results, that showed a reduction in anxiety symptoms.
Non-probiotic interventions were also more effective in the studies that used IRIF alone.
In those studies only using IRIF, 80% were effective when using non-probiotic interventions, while only 45% were found to be effective when using probiotic ways.
The authors said one reason that non-probiotic interventions were significantly more effective than probiotic interventions was possibly due to the fact that changing diet (a diverse energy source) could have more of an impact on gut bacteria growth than introducing specific types of bacteria in a probiotic supplement.
Also, because some studies had involved introducing different types of probiotics, these could have fought against each other to work effectively, and many of the intervention times used might have been too short to significantly increase the abundance of the imported bacteria.
Most of the studies did not report serious adverse events, and only four studies reported mild adverse effects such as dry mouth and diarrhea.
This is an observational study, and as such, cannot establish cause. Indeed, the authors acknowledged some limitations, such as differences in study design, subjects, interventions and measurements, making the data unsuitable for further analysis.
Nevertheless, they said the overall quality of the 21 studies included was high.
The researchers concluded: “We find that more than half of the studies included showed it was positive to treat anxiety symptoms by regulation of intestinal microbiota.
“There are two kinds of interventions (probiotic and non-probiotic interventions) to regulate intestinal microbiota, and it should be highlighted that the non-probiotic interventions were more effective than the probiotic interventions. More studies are needed to clarify this conclusion since we still cannot run meta-analysis so far.”
They also suggested that, in addition to the use of psychiatric drugs for treatment, “we can also consider regulating intestinal flora to alleviate anxiety symptoms.”