By Kristina Campbell, Contributing Writer06.03.19
Human milk is unlike any other kind of milk. It is a chemical marvel: a nutrient-dense substance with constantly-changing ratios of fats and immunologically active components (Ballard & Morrow, 2013). Most importantly, it’s chock full of unique sugars called human milk oligosaccharides (HMOs) that have complex, highly diverse structures (Bode, 2012).
HMOs are known to support infant health—and they do so through several different mechanisms, but most notably by shaping gut microbiota development. Because of recent food science innovations, it has become possible to add these unique carbohydrates to infant formula; and with the cutting-edge tools now at hand, scientists will increasingly be able to uncover how HMOs affect the gut microbiota and health, bringing new focus to the search for infant nutritional products that support optimal health.
A Mystery Substance
It was through the study of infant gut bacteria that HMOs were identified and named in the first place. Pediatricians in the late 1800s were investigating how infants’ intestinal bacteria influenced their physiology, and by the 1920s it was clear that human breast milk contained a mystery substance that promoted the growth of bifidobacteria in the digestive tract—a “bifidus factor.” In parallel, chemists had been studying the carbohydrates that were highly abundant in human milk (as compared to cow’s milk) and had identified a unique carbohydrate fraction called gynolactose. In 1954 the work of these groups converged, landing on oligosaccharides as the unknown “bifidus factor” in human breast milk (Bode, 2012). Around 99% of ingested HMOs were excreted in the infant’s feces, which made perfect sense: HMOs were food not for the infant itself, but for the microorganisms living in the infant’s digestive tract.
As the pediatricians knew, the growth of bacteria in the gut was not an end in itself. Although the HMOs fed bacteria that were widely considered beneficial, a stronger link needed to be made between specific bugs and infant health or disease. The tools to make this happen would emerge in the following decades.
The Community Context
When culture-independent methods (such as 16S rRNA gene sequencing and shotgun metagenomic sequencing) became practical for microbiologists’ use at the end of the 20th century, scientific advancements began to place knowledge about infant bifidobacteria into the broader context of the gut microbiota: in other words, the entire collection of microorganisms (bacteria as well as archaea and eukaryotes) present in the digestive tract. With the newfound ability to take a “snapshot” of the overall bacterial community at a point in time, it became possible for researchers to investigate how both specific bacteria and the overall bacterial community of the infant related to measurable health outcomes.
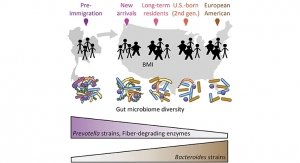
A picture emerged of the gut microbiota in early life: scientists discovered that during the birth process, vaginally born infants are colonized by microbes from the birth canal, while those born by caesarean section are initially colonized by microbes on adults’ skin and on hospital surfaces (Dominguez-Bello et al., 2010). After these first exposures, healthy infants tend to have a gut microbiota dominated by bifidobacterium species, with low diversity—unlike later in life, when greater diversity is associated with good health. And throughout the first months of life, diet is one of the biggest contributors to what a baby’s gut microbial community looks like.
Sure enough, HMOs had dramatic effects on this ecologically complex community of microorganisms. The gut microbiota of breastfed babies was found to differ from those who were formula fed, with an increase in HMO-consuming bacteria from the families Bacteroidaceae and Bifidobacteriaceae in breastfed infants (De Leoz et al., 2015). Corroborating this was the fact that gut bacterial species were differently equipped to use HMOs: while almost all strains of Bifidobacterium longum subsp. infantis (or B. infantis) were efficient at using diverse HMOs as a metabolic substrate, not all strains of B. bifidum were equipped for the same (Garrido et al., 2015). HMOs appeared to be consumed by very specific bacteria, which shaped the overall gut microbiota composition—not trivially, since this was occurring at an important time in the development of the infant immune system (Seppo et al., 2019).
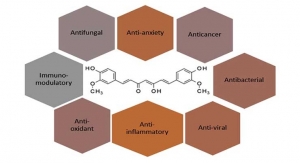
Scientists from diverse disciplines continued to investigate the secrets of HMOs over time. Overall, it’s clear that HMOs support the health of infants: protecting against certain newborn infections, reducing the risk of allergies and inflammation, and promoting brain development and neuronal activity. Certainly, HMO-bacteria interactions may be important for some of these health effects; but in other cases, the mechanisms may be completely different. For instance, HMOs appear able to modify gene expression in intestinal epithelial cells, leading to changes in some cell responses (Bode, 2012), an effect that does not necessarily rely on gut microbiota.
Toward Better Infant Nutrition
Today, over 200 HMOs have been identified—each one a uniquely structured molecule. And although HMO-rich human breast milk is the best possible nutrition for an infant, the reality is that many women have a reduced ability to breastfeed and are looking for alternatives that support the health of their infants.
Science had uncovered the value of HMOs for infant health long before it was possible to produce them in sufficient quantities for inclusion in infant formula. So instead, the more common fructo-oligosaccharides (FOS) and galacto-oligosaccharides (GOS) were often included in infant formula as an HMO substitute. These functional ingredients in infant formula appear to spur the growth of bifidobacteria and successfully alter the gastrointestinal microbiota of formula-fed babies to resemble that of breastfed ones; but the chemical structures of these substances are ultimately very different from HMOs—with straighter, rather than more branched structures—and evidence for their health benefits (especially long-term) is somewhat limited (Vandenplas, De Greef, & Veereman, 2014).
Meanwhile, producing HMOs in great enough quantities for inclusion in functional foods was a technical challenge that scientists were working to overcome.
Breakthroughs in HMO Production
Leading companies met the challenge head-on. Katja Parschat, deputy head of R&D at Jennewein Biotechnologie, a German company founded in 2005, said innovation began in earnest in the 1990s. “Some companies tried to create HMOs by chemical synthesis,” she explained. “It is possible, but it is very elaborate and very costly.”
Fermentation, on the other hand, simplified the process of creating HMOs by getting bacteria to do the work; it was a robust, safe method that made use of specific bacterial species like engineered Escherichia coli. “If you get a really effective bacterial system, you can produce HMOs on a large scale,” Parschat noted.
She described the company’s approach: “We are using genetically modified organisms—bacteria—that are able to produce single HMOs. We engineered them by introducing genes like transferases, enzymes that catalyze specific reactions, and have modified them so that efficiency for HMO production is getting better and better.” She said that a fermentation in inexpensive media can yield high titers of HMOs, with the HMOs being easy to separate from the supernatant afterward.
“We started with 2’-fucosyllactose when we started with production of HMOs, because 2’-fucosyllactose is the most abundant HMO in the breast milk of over 80% of women globally,” Parschat said.
New Connections to Health: The Gut Microbiota
Now that HMO-rich formula exists, the conditions are ideal for a new era in infant nutrition: available tools for studying the complex infant gut microbiota, plus the technological capabilities for producing HMOs and adding them in specific combinations to infant formula.
The key will be to link HMOs to more specific clinical outcomes, both short-term and long-term, through the infant gut microbiota. Scientists speculate that perhaps the HMO intake of formula-fed babies could be directed to improve health or mitigate disease through the microbiota. Or HMOs could be combined with probiotics (creating tailored “synbiotics”) to achieve predefined functional outcomes (Garrido et al., 2015). According to American microbiome scientist Rob Knight, it may one day be possible to monitor babies’ microbiota in early life, and using a “microbiome GPS” system (“Big Data from World’s Largest Citizen Science Microbiome Project Serves Food for Thought”), health professionals would know which gut microbial community is supportive of health and what mixture of HMOs and/or probiotics would change the complex ecology of the gut in order to arrive there.
All this advancement occurs in a milieu where the gut microbiota is a “trending” topic, not only among the scientists themselves, but also among the general public. High consumer interest sets the stage for widespread learning about the benefits of HMOs for infant health through the microbiota, opening up new ways of delivering infant nutrition and monitoring its effects on health.
Kristina Campbell is a well-known Canadian science writer specializing in the gut microbiota, digestive health, and nutrition. She has also authored two books: “The Well-Fed-Microbiome Cookbook” and “Gut Microbiota: Interactive Effects on Nutrition and Health.” Jennewein Biotechnologie specializes in the production of rare functional monosaccharides and oligosaccharides for nutritional, pharmaceutical, cosmetic, and medical applications. It manufactures a portfolio of human milk oligosaccharides that are produced using fermentation technology. For more information, contact Bettina Gutiérrez, Bettina.gutierrez@jennewein-biotech.de; www.jennewein-biotech.de/en.
References
HMOs are known to support infant health—and they do so through several different mechanisms, but most notably by shaping gut microbiota development. Because of recent food science innovations, it has become possible to add these unique carbohydrates to infant formula; and with the cutting-edge tools now at hand, scientists will increasingly be able to uncover how HMOs affect the gut microbiota and health, bringing new focus to the search for infant nutritional products that support optimal health.
A Mystery Substance
It was through the study of infant gut bacteria that HMOs were identified and named in the first place. Pediatricians in the late 1800s were investigating how infants’ intestinal bacteria influenced their physiology, and by the 1920s it was clear that human breast milk contained a mystery substance that promoted the growth of bifidobacteria in the digestive tract—a “bifidus factor.” In parallel, chemists had been studying the carbohydrates that were highly abundant in human milk (as compared to cow’s milk) and had identified a unique carbohydrate fraction called gynolactose. In 1954 the work of these groups converged, landing on oligosaccharides as the unknown “bifidus factor” in human breast milk (Bode, 2012). Around 99% of ingested HMOs were excreted in the infant’s feces, which made perfect sense: HMOs were food not for the infant itself, but for the microorganisms living in the infant’s digestive tract.
As the pediatricians knew, the growth of bacteria in the gut was not an end in itself. Although the HMOs fed bacteria that were widely considered beneficial, a stronger link needed to be made between specific bugs and infant health or disease. The tools to make this happen would emerge in the following decades.
The Community Context
When culture-independent methods (such as 16S rRNA gene sequencing and shotgun metagenomic sequencing) became practical for microbiologists’ use at the end of the 20th century, scientific advancements began to place knowledge about infant bifidobacteria into the broader context of the gut microbiota: in other words, the entire collection of microorganisms (bacteria as well as archaea and eukaryotes) present in the digestive tract. With the newfound ability to take a “snapshot” of the overall bacterial community at a point in time, it became possible for researchers to investigate how both specific bacteria and the overall bacterial community of the infant related to measurable health outcomes.
A picture emerged of the gut microbiota in early life: scientists discovered that during the birth process, vaginally born infants are colonized by microbes from the birth canal, while those born by caesarean section are initially colonized by microbes on adults’ skin and on hospital surfaces (Dominguez-Bello et al., 2010). After these first exposures, healthy infants tend to have a gut microbiota dominated by bifidobacterium species, with low diversity—unlike later in life, when greater diversity is associated with good health. And throughout the first months of life, diet is one of the biggest contributors to what a baby’s gut microbial community looks like.
Sure enough, HMOs had dramatic effects on this ecologically complex community of microorganisms. The gut microbiota of breastfed babies was found to differ from those who were formula fed, with an increase in HMO-consuming bacteria from the families Bacteroidaceae and Bifidobacteriaceae in breastfed infants (De Leoz et al., 2015). Corroborating this was the fact that gut bacterial species were differently equipped to use HMOs: while almost all strains of Bifidobacterium longum subsp. infantis (or B. infantis) were efficient at using diverse HMOs as a metabolic substrate, not all strains of B. bifidum were equipped for the same (Garrido et al., 2015). HMOs appeared to be consumed by very specific bacteria, which shaped the overall gut microbiota composition—not trivially, since this was occurring at an important time in the development of the infant immune system (Seppo et al., 2019).
Scientists from diverse disciplines continued to investigate the secrets of HMOs over time. Overall, it’s clear that HMOs support the health of infants: protecting against certain newborn infections, reducing the risk of allergies and inflammation, and promoting brain development and neuronal activity. Certainly, HMO-bacteria interactions may be important for some of these health effects; but in other cases, the mechanisms may be completely different. For instance, HMOs appear able to modify gene expression in intestinal epithelial cells, leading to changes in some cell responses (Bode, 2012), an effect that does not necessarily rely on gut microbiota.
Toward Better Infant Nutrition
Today, over 200 HMOs have been identified—each one a uniquely structured molecule. And although HMO-rich human breast milk is the best possible nutrition for an infant, the reality is that many women have a reduced ability to breastfeed and are looking for alternatives that support the health of their infants.
Science had uncovered the value of HMOs for infant health long before it was possible to produce them in sufficient quantities for inclusion in infant formula. So instead, the more common fructo-oligosaccharides (FOS) and galacto-oligosaccharides (GOS) were often included in infant formula as an HMO substitute. These functional ingredients in infant formula appear to spur the growth of bifidobacteria and successfully alter the gastrointestinal microbiota of formula-fed babies to resemble that of breastfed ones; but the chemical structures of these substances are ultimately very different from HMOs—with straighter, rather than more branched structures—and evidence for their health benefits (especially long-term) is somewhat limited (Vandenplas, De Greef, & Veereman, 2014).
Meanwhile, producing HMOs in great enough quantities for inclusion in functional foods was a technical challenge that scientists were working to overcome.
Breakthroughs in HMO Production
Leading companies met the challenge head-on. Katja Parschat, deputy head of R&D at Jennewein Biotechnologie, a German company founded in 2005, said innovation began in earnest in the 1990s. “Some companies tried to create HMOs by chemical synthesis,” she explained. “It is possible, but it is very elaborate and very costly.”
Fermentation, on the other hand, simplified the process of creating HMOs by getting bacteria to do the work; it was a robust, safe method that made use of specific bacterial species like engineered Escherichia coli. “If you get a really effective bacterial system, you can produce HMOs on a large scale,” Parschat noted.
She described the company’s approach: “We are using genetically modified organisms—bacteria—that are able to produce single HMOs. We engineered them by introducing genes like transferases, enzymes that catalyze specific reactions, and have modified them so that efficiency for HMO production is getting better and better.” She said that a fermentation in inexpensive media can yield high titers of HMOs, with the HMOs being easy to separate from the supernatant afterward.
“We started with 2’-fucosyllactose when we started with production of HMOs, because 2’-fucosyllactose is the most abundant HMO in the breast milk of over 80% of women globally,” Parschat said.
New Connections to Health: The Gut Microbiota
Now that HMO-rich formula exists, the conditions are ideal for a new era in infant nutrition: available tools for studying the complex infant gut microbiota, plus the technological capabilities for producing HMOs and adding them in specific combinations to infant formula.
The key will be to link HMOs to more specific clinical outcomes, both short-term and long-term, through the infant gut microbiota. Scientists speculate that perhaps the HMO intake of formula-fed babies could be directed to improve health or mitigate disease through the microbiota. Or HMOs could be combined with probiotics (creating tailored “synbiotics”) to achieve predefined functional outcomes (Garrido et al., 2015). According to American microbiome scientist Rob Knight, it may one day be possible to monitor babies’ microbiota in early life, and using a “microbiome GPS” system (“Big Data from World’s Largest Citizen Science Microbiome Project Serves Food for Thought”), health professionals would know which gut microbial community is supportive of health and what mixture of HMOs and/or probiotics would change the complex ecology of the gut in order to arrive there.
All this advancement occurs in a milieu where the gut microbiota is a “trending” topic, not only among the scientists themselves, but also among the general public. High consumer interest sets the stage for widespread learning about the benefits of HMOs for infant health through the microbiota, opening up new ways of delivering infant nutrition and monitoring its effects on health.
Kristina Campbell is a well-known Canadian science writer specializing in the gut microbiota, digestive health, and nutrition. She has also authored two books: “The Well-Fed-Microbiome Cookbook” and “Gut Microbiota: Interactive Effects on Nutrition and Health.” Jennewein Biotechnologie specializes in the production of rare functional monosaccharides and oligosaccharides for nutritional, pharmaceutical, cosmetic, and medical applications. It manufactures a portfolio of human milk oligosaccharides that are produced using fermentation technology. For more information, contact Bettina Gutiérrez, Bettina.gutierrez@jennewein-biotech.de; www.jennewein-biotech.de/en.
References
- Ballard, O., & Morrow, A. L. (2013). Human milk composition: nutrients and bioactive factors. Pediatric Clinics of North America, 60(1), 49–74. https://doi.org/10.1016/j.pcl.2012.10.002
- Big Data from World’s Largest Citizen Science Microbiome Project Serves Food for Thought. (n.d.). Retrieved May 4, 2019, from https://health.ucsd.edu/news/releases/pages/2018-05-15-big-data-from-worlds-largest-citizen-science-microbiome-project-serves-food-for-thought.aspx
- Bode, L. (2012). Humtan milk oligosaccharides: every baby needs a sugar mama. Glycobiology, 22(9), 1147–1162. https://doi.org/10.1093/glycob/cws074
- De Leoz, M. L. A., Kalanetra, K. M., Bokulich, N. A., Strum, J. S., Underwood, M. A., German, J. B., … Lebrilla, C. B. (2015). Human Milk Glycomics and Gut Microbial Genomics in Infant Feces Show a Correlation between Human Milk Oligosaccharides and Gut Microbiota: A Proof-of-Concept Study. Journal of Proteome Research, 14(1), 491–502. https://doi.org/10.1021/pr500759e
- Dominguez-Bello, M. G., Costello, E. K., Contreras, M., Magris, M., Hidalgo, G., Fierer, N., & Knight, R. (2010). Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proceedings of the National Academy of Sciences of the United States of America, 107(26), 11971–11975. https://doi.org/10.1073/pnas.1002601107
- Garrido, D., Ruiz-Moyano, S., Lemay, D. G., Sela, D. A., German, J. B., & Mills, D. A. (2015). Comparative transcriptomics reveals key differences in the response to milk oligosaccharides of infant gut-associated bifidobacteria. Scientific Reports, 5(1), 13517. https://doi.org/10.1038/srep13517
- Seppo, A. E., Kukkonen, A. K., Kuitunen, M., Savilahti, E., Yonemitsu, C., Bode, L., & Järvinen, K. M. (2019). Association of Maternal Probiotic Supplementation With Human Milk Oligosaccharide Composition. JAMA Pediatrics, 173(3), 286. https://doi.org/10.1001/jamapediatrics.2018.4835
- Vandenplas, Y., De Greef, E., & Veereman, G. (2014). Prebiotics in infant formula. Gut Microbes, 5(6), 681–687. https://doi.org/10.4161/19490976.2014.972237