By Dilip Ghosh, PhD, FACN, nutriConnect10.01.18
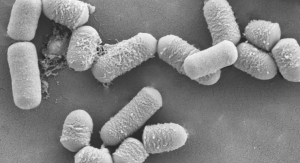
Major depressive disorder (MDD), including mood oscillation and anxiety, is the leading psychiatric disorder worldwide, resulting in significant economic and emotional costs. Treatment is still challenging, as one in two patients do not respond adequately to treatment or relapse over time. Recently, the gut microbiome has been proposed to play a significant role in prognosis of pathological levels of depression.
It is now well established that gut colonizers mediate the effects of early life events on adult behavior. This is also linked to activation of the “hypothalamic–pituitary–adrenal” axis, which in turn impacts the gut via the enteric nervous system. Beneficial effects may include developing the immune and central nervous systems, which extract nutrients from food and keep harmful microbes away. This bidirectional communication between the microbiota and the CNS occurs through autonomic, neuroendocrine, enteric, and immune system pathways.
Key Findings
Accumulating evidence from human and animal studies suggests a role for the gut microbiota in brain function, including for anxiety and mood disorders. Key findings have suggested:
It is not surprising that nutrition and depression are linked, as food consumed can significantly change the composition of the microbiota. A recent study indicated that alterations in the microbiota composition elicited by nutrition are associated with altered neurotransmitter concentrations, which in turn are linked to cognitive impairments. Nutrient-poor, energy-dense, processed foods influence hormonal, neurotransmitter, and signaling pathways, which in turn modulate several brain processes impacting both appetite and mood.
Conclusion
We are still at a very early stage of understanding the complex role of gut microbes and how they regulate immune function, adaptive stress response, and ultimately, brain function and behavior. The potential role of various treatments (e.g., probiotics, antibiotics, fecal microbiota transplantation) in altering the composition of the gut microbiota for the prevention and treatment of various psychiatric disorders, such as depression and anxiety, are under investigation. We now await future translation into controlled human clinical investigations and the results of large-scale placebo-controlled trials.
References
Dilip Ghosh, PhD, FACN
nutriConnect
About the author: Dilip Ghosh, PhD, FACN, is director of nutriConnect, based in Sydney, Australia. He is also professionally involved with NICM, Western Sydney University, Australia, and is an Honorary Ambassador with the Global Harmonization Initiative (GHI). Dr. Ghosh received his PhD in biomedical science from University of Calcutta, India. He has been involved in drug development (both synthetic and natural) and functional food research and development both in academic and industry domains. Dr. Ghosh has published more than 90 papers in peer-reviewed journals, and he has authored many books, including: “Biotechnology in Functional Foods and Nutraceuticals,” “Innovation in Healthy and Functional Foods,” “Clinical Perspective of Functional Foods and Nutraceuticals,” and “Pharmaceuticals to Nutraceuticals: A Shift in Disease Prevention under CRC Press. He can be reached at dghosh@optusnet.com.au; www.nutriconnect.com.au.
It is now well established that gut colonizers mediate the effects of early life events on adult behavior. This is also linked to activation of the “hypothalamic–pituitary–adrenal” axis, which in turn impacts the gut via the enteric nervous system. Beneficial effects may include developing the immune and central nervous systems, which extract nutrients from food and keep harmful microbes away. This bidirectional communication between the microbiota and the CNS occurs through autonomic, neuroendocrine, enteric, and immune system pathways.
Key Findings
Accumulating evidence from human and animal studies suggests a role for the gut microbiota in brain function, including for anxiety and mood disorders. Key findings have suggested:
- “Leaky gut hypothesis” of MDD links inflammation and gut microbiota to depression.
- Gut microbiota impacts depression development via serotonergic systems.
- Interventions targeting the microbiota are promising tools to modulate depression.
It is not surprising that nutrition and depression are linked, as food consumed can significantly change the composition of the microbiota. A recent study indicated that alterations in the microbiota composition elicited by nutrition are associated with altered neurotransmitter concentrations, which in turn are linked to cognitive impairments. Nutrient-poor, energy-dense, processed foods influence hormonal, neurotransmitter, and signaling pathways, which in turn modulate several brain processes impacting both appetite and mood.
Conclusion
We are still at a very early stage of understanding the complex role of gut microbes and how they regulate immune function, adaptive stress response, and ultimately, brain function and behavior. The potential role of various treatments (e.g., probiotics, antibiotics, fecal microbiota transplantation) in altering the composition of the gut microbiota for the prevention and treatment of various psychiatric disorders, such as depression and anxiety, are under investigation. We now await future translation into controlled human clinical investigations and the results of large-scale placebo-controlled trials.
References
- Koopman M et al. 2017. Depressed gut? The microbiota-diet-inflammation trialogue in depression. Curr Opin Psychiatry, 30:369–377.
- Noble EE, et al. 2017. Gut to Brain dysbiosis: mechanisms linking western diet consumption, the microbiome, and cognitive impairment. Front Behav Neurosci, 11:9.
- Rieder R et al. 2017. Microbes and mental health: A review. Brain, Behavior, and Immunity, 66: 9–17
Dilip Ghosh, PhD, FACN
nutriConnect
About the author: Dilip Ghosh, PhD, FACN, is director of nutriConnect, based in Sydney, Australia. He is also professionally involved with NICM, Western Sydney University, Australia, and is an Honorary Ambassador with the Global Harmonization Initiative (GHI). Dr. Ghosh received his PhD in biomedical science from University of Calcutta, India. He has been involved in drug development (both synthetic and natural) and functional food research and development both in academic and industry domains. Dr. Ghosh has published more than 90 papers in peer-reviewed journals, and he has authored many books, including: “Biotechnology in Functional Foods and Nutraceuticals,” “Innovation in Healthy and Functional Foods,” “Clinical Perspective of Functional Foods and Nutraceuticals,” and “Pharmaceuticals to Nutraceuticals: A Shift in Disease Prevention under CRC Press. He can be reached at dghosh@optusnet.com.au; www.nutriconnect.com.au.