06.30.20
While vitamin K1 and K2 are considered to be very distinct due to the differences in health benefits that each respective member of the K family offers, a recent study published in the American Journal of Clinical Nutrition conducted by researchers at Tufts University and Tufts Medical Center suggests that vitamin K1 in the form of phylloquinone has its own protective benefits associated with all-cause mortality.
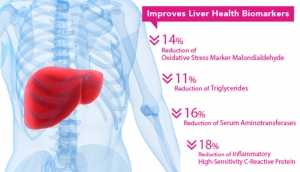
Vascular tissues contains vitamin K dependent proteins, though research suggests that the activity of K1 is mostly confined to the K-dependent proteins in the liver, whereas K2 is believed to function much more actively throughout the cardiovascular system to prevent vascular calcification.
The protective effect that K1 has, however, should not be underestimated. The authors of the meta-analysis found that in three cohorts of Americans, amounting to a total study population of 4,000 adults between the ages of 54 and 76, those with the greatest deficiencies in vitamin K1 had a 19 percent higher risk of death compared to those who had a sufficient K1 intake. Still, the research did not associated low K1 levels with CVD.
The study participants were sourced from the Health, Aging, and Body Composition Study, the Multi-Ethnic Study of Atherosclerosis, and the Framingham Offspring Study, known cohorts with available measures of fasting circulating phylloquinone (vitamin K1) and confirmed CBD events and mortality, as measured by fasting blood samples.
A statistical model found an association between circulating phylloquinone with incident CVD and all-cause mortality risk, while taking other health factors, such as diet, exercise, smoking and more, into account.
In the overall population, there were 858 CVD incidents and 1209 deaths over a median of 13 years.
The authors of the meta-analysis concluded that the association between vitamin K1 deficiency and all-cause mortality warrants further studies to clarify the mechanism underlying the protective benefits they uncovered through the analysis, and, furthermore, to evaluate the impact of increased K1 intake on cardiovascular and other health outcomes in individuals with low vitamin K status. The conclusion, ultimately, is observational, as no mechanism has been identified to explain why circulating vitamin K1 was associated with a reduced risk for death but not heart disease.
Vascular tissues contains vitamin K dependent proteins, though research suggests that the activity of K1 is mostly confined to the K-dependent proteins in the liver, whereas K2 is believed to function much more actively throughout the cardiovascular system to prevent vascular calcification.
The protective effect that K1 has, however, should not be underestimated. The authors of the meta-analysis found that in three cohorts of Americans, amounting to a total study population of 4,000 adults between the ages of 54 and 76, those with the greatest deficiencies in vitamin K1 had a 19 percent higher risk of death compared to those who had a sufficient K1 intake. Still, the research did not associated low K1 levels with CVD.
The study participants were sourced from the Health, Aging, and Body Composition Study, the Multi-Ethnic Study of Atherosclerosis, and the Framingham Offspring Study, known cohorts with available measures of fasting circulating phylloquinone (vitamin K1) and confirmed CBD events and mortality, as measured by fasting blood samples.
A statistical model found an association between circulating phylloquinone with incident CVD and all-cause mortality risk, while taking other health factors, such as diet, exercise, smoking and more, into account.
In the overall population, there were 858 CVD incidents and 1209 deaths over a median of 13 years.
The authors of the meta-analysis concluded that the association between vitamin K1 deficiency and all-cause mortality warrants further studies to clarify the mechanism underlying the protective benefits they uncovered through the analysis, and, furthermore, to evaluate the impact of increased K1 intake on cardiovascular and other health outcomes in individuals with low vitamin K status. The conclusion, ultimately, is observational, as no mechanism has been identified to explain why circulating vitamin K1 was associated with a reduced risk for death but not heart disease.